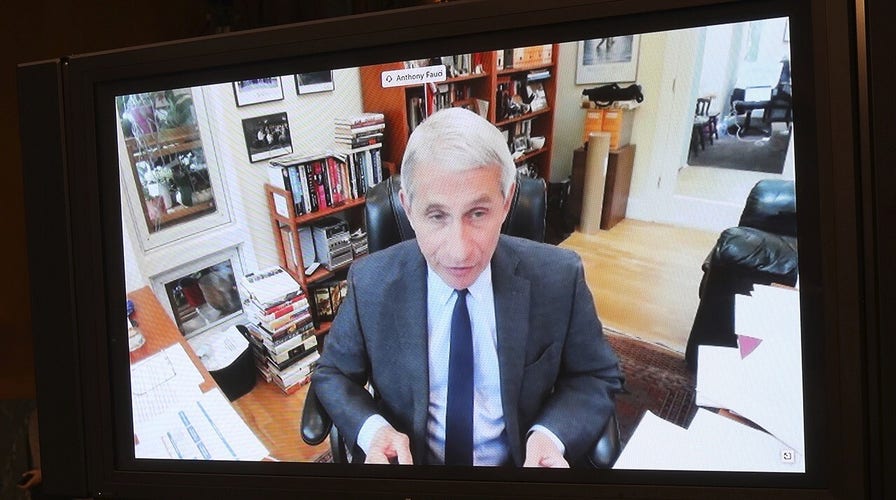
Fauci addresses measures to protect nursing homes at Senate hearing
Dr. Nicole Saphier reacts to the testimony on COVID-19 on 'Outnumbered.'
Get all the latest news on coronavirus and more delivered daily to your inbox. Sign up here.
While only 1.6 percent of the U.S. population – 5.1 million people as of 2016 – lives in nursing homes and other residential care facilities, an estimated 40 percent of deaths from COVID-19 have occurred in these facilities, excluding the New York City area.
The dramatically disproportionate death toll from the disease caused by the novel coronavirus in nursing homes holds true in many countries around the world.
Researchers at the International Long Term Care Policy Network report that in Australia, Belgium, Canada, Denmark, France, Germany, Hong Kong, Hungary, Ireland, Israel, Norway, Portugal, Singapore, and Sweden, 49.4 percent of reported COVID-19 death have taken place in nursing homes.
These statistics make it obvious that we need to pay special attention to protecting nursing home residents to help reduce the terrible death toll the coronavirus pandemic is taking. As of Saturday, the confirmed death toll from the pandemic in the U.S. topped 87,000 people.
Nursing home neglect is a tragic but common occurrence in our country. Although elder abuse can happen from in-home care as well, it all too often occurs when caregivers feel overworked and exhausted.
More from Opinion
Since reports of negligent and substandard care at any nursing homes across the country show this is a serious problem, this may be the time for Congress to consider the importance of adequate staffing and compensation for long-term care facility employees – as well as transitioning some of our elderly and disabled to in-home care settings.
Policy implications moving forward must pay significant attention to infections in assisted-living facilities, especially focusing on staff who work at multiple sites, patients coming directly from the hospital and visitors to the facilities.
As I discuss in my book, “Make America Healthy Again,” while our medical advancements have provided us with a longer lifespan, many elderly Americans are living with diseases and medical conditions that make them especially susceptible to the most severe effects of COVID-19.
“Our increased longevity is one of the greatest medical achievements of the modern era,” I wrote in my book. “On average, Americans today can expect to live nearly thirty years longer than did our predecessors at the turn of the twentieth century…. As medical advancements continue to improve health, and more baby boomers enter their retirement years, the demand for long-term medical services is growing.”
According to the Alzheimer’s Association, nearly 5.7 million people in the U.S. are living with dementia. Similar to the global trends, these numbers are expected to rise as life expectancy increases.
Additionally, almost all recipients of Medicare with dementia (95 percent) have at least one other preexisting chronic health condition. And because of their impaired memory and reasoning ability, people living with dementia cannot solely manage or direct their own care. This requires them to live with a caregiver or in an assisted-living facility.
According to Robert Egge, chief public policy office of the Alzheimer’s Association: “While there is a significant number of priority actions to take during a global pandemic like this, it has been increasingly clear that nursing homes and other long-term care communities are ‘hot spots’ for COVID-19. And their residents with dementia are particularly susceptible due to their age, their increased likelihood of coexisting chronic conditions, and the community nature of these settings. These issues have likely been overlooked due to an inability to access the necessary testing and inaccurate reporting. There is an urgent need, and there has been for some time, to address the disproportionate vulnerability of this population.”
The Alzheimer’s Association is urging policymakers to implement new policy solutions that will address the immediate and long-term issues impacting care facilities during the COVID-19 pandemic, including:
Testing
Each nursing home and assisted living community should have the onsite capability to verify that all residents, staff and visitors are free of COVID-19 infection, whether or not they are symptomatic.
Access to testing should be the “White House Standard,” where staff members are tested frequently. Government support is needed to ensure accelerated production and delivery of testing material to nursing homes, with rapid turnaround testing staffed by trained personnel.
Reporting
All cases of COVID-19 at nursing homes and assisted living communities need to be reported immediately and accurately.
Additionally, these reports should be updated upon remission, death, transfer or other appropriate status update. With all appropriate privacy safeguards for individuals, this reported data should be freely and immediately accessible to all, down to the facility level.
Surge Activation
As “hot spots” occur, they must be dealt with urgently and effectively. Any reported cases should trigger careful, ongoing monitoring. If conditions warrant, “strike teams” should be employed to a facility to provide needed support until the outbreak is appropriately contained and eliminated.
Personal Protective Equipment (PPE)
All nursing homes and assisted living communities should have full access to all needed PPE, testing equipment, training and external support to keep them COVID-19 free.
Sharply increased unemployment and other economic fallout caused by measures to slow the spread of COVID-19 are taking an increasing toll on the mental and financial health of the American people.
Almost all states around the nation are at least partially lifting stay-at-home orders and restrictions on businesses because officials realize we can’t continue to keep our country locked down for months or perhaps even years while we await the availability of a coronavirus vaccine and effective treatments for COVID-19.
As a result, state and federal officials must ensure that measures are in place to protect the most vulnerable people in our country while we reopen.
As the statistics on COVID-19 deaths in nursing homes make clear, the risk of death from this new disease is not spread evenly across our population.
Some 94 percent of our nation’s workforce is under age 55, and those without serious medical conditions are at far lower risk of dying from COVID-19 than are elderly Americans. In addition, children having the lowest severity profile of COVID-19 deaths.
So it makes sense that if we can focus on protecting the most vulnerable among us, our country can regain a level of normalcy while carefully reopening.
A crucial mission will be to limit asymptomatic spread amongst the elderly, near-elderly and those with preexisting conditions. There is little doubt that even under the best of circumstances, when stay-at-home orders are loosened (as they should be), there will be increased COVID-19 cases.
CLICK HERE TO SIGN UP FOR OUR OPINION NEWSLETTER
What’s important is whether we are capable of identifying and reporting new cases and decreasing the amount of virus transmission.
The good news is that officials at every level of government have the information to strategically reopen our country by acknowledging the fact that the elderly and the near-elderly who also have other chronic diseases are at the greatest risk of deaths and severe illness caused by COVID-19.
The key to moving forward is ensuring that nursing homes and assisted-care facilities have adequate PPE supplies, universal access to perform enhanced surveillance and point-of-care testing, reporting measures in place, and protocols listed for new COVID-19 case surges.
Additionally, as “excess deaths” in the home setting are reported, ensuring the safety of the most vulnerable Americans being cared for at home would only be feasible if caregivers were provided the necessary resources to care for their family members at home.
CLICK HERE TO GET THE FOX NEWS APP
Investing more resources so that nursing homes are better-positioned to respond to and contain virus outbreaks won’t eliminate the threat posed by COVID-19 and other viral diseases, but it could significantly reduce the death toll of these diseases.
If the coronavirus pandemic results in increased safety and hygiene measures throughout our nation’s nursing homes – and increased home-care resources for our elderly and disabled with the closure of facilities providing substandard care – we will be able to save lives and be better prepared to deal with viral diseases far into the future.