Funded Studies Details

The first survivor of Alzheimer's is out there, but we won't get there without you.
Donate Now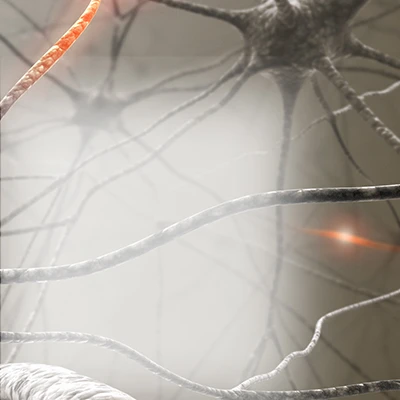
Learn how Alzheimer’s disease affects the brain.
Take the Brain Tour
