Quick facts
Nearly 7 million Americans are living with Alzheimer's. By 2050, this number is projected to rise to nearly 13 million.

Alzheimer's disease was the fifth-leading cause of death among people age 65 and older in 2021.

Health and long-term care costs for people living with dementia are projected to reach $360 billion in 2024 and nearly $1 trillion in 2050.
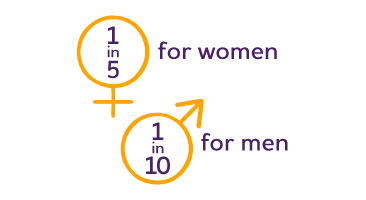
The lifetime risk for Alzheimer's at age 45 is 1 in 5 for women and 1 in 10 for men.

Over 11 million Americans provide unpaid care for people with Alzheimer's or other dementias.

In 2023, unpaid caregivers provided an estimated 18.4 billion hours of care valued at nearly $350 billion.

70% of dementia caregivers say that coordinating care is stressful. Two-thirds also have difficulty finding resources and support for their needs.

74% of dementia caregivers say that they are concerned about maintaining their own health since becoming a caregiver.

60% of health care workers believe that the U.S. health care system is not effectively helping patients and their families navigate dementia care.
Prevalence
 The number of Americans living with Alzheimer's is growing — and growing fast. Nearly 7 million Americans have Alzheimer's.
The number of Americans living with Alzheimer's is growing — and growing fast. Nearly 7 million Americans have Alzheimer's.
- An estimated 6.9 million Americans age 65 and older are living with Alzheimer's in 2024. Seventy-three percent are age 75 or older.
- About 1 in 9 people age 65 and older (10.9%) has Alzheimer's.
- Almost two-thirds of Americans with Alzheimer's are women.
- Older Black Americans are about twice as likely to have Alzheimer's or other dementias as older Whites.
- Older Hispanics are about one and one-half times as likely to have Alzheimer's or other dementias as older Whites.
As the size of the U.S. population age 65 and older continues to grow, so too will the number and proportion of Americans with Alzheimer's or other dementias. By 2050, the number of people age 65 and older with Alzheimer's may grow to a projected 12.7 million, barring the development of medical breakthroughs to prevent or cure Alzheimer's disease.
Get involved
Volunteer, fundraise, advocate and more — you can make a difference in the lives of people affected by Alzheimer's.
Mortality and morbidity
 Alzheimer's is not just memory loss. Alzheimer's kills.
Alzheimer's is not just memory loss. Alzheimer's kills.
- One in 3 seniors dies with Alzheimer's or another dementia. It kills more than breast cancer and prostate cancer combined.
- Deaths from Alzheimer's have more than doubled between 2000 and 2021, while those from heart disease — the leading cause of death — have decreased.
- At age 70, seniors living with Alzheimer's are twice as likely to die before age 80 than those who do not have the disease.
People age 65 and older survive an average of four to eight years after a diagnosis of Alzheimer's, yet some live as long as 20 years with Alzheimer's. This reflects the slow, uncertain progression of the disease.
Invest in the fight to end Alzheimer's
The first survivor of Alzheimer's is out there, but we won’t get there without you.
Caregiving
 Eighty-three percent of the help provided to older adults in the United States comes from family members, friends or other unpaid caregivers. Nearly half of all caregivers who provide help to older adults do so for someone living with Alzheimer's or another dementia.
Eighty-three percent of the help provided to older adults in the United States comes from family members, friends or other unpaid caregivers. Nearly half of all caregivers who provide help to older adults do so for someone living with Alzheimer's or another dementia.
Who are the caregivers?
- About 30% of caregivers are age 65 or older.
- Approximately two-thirds of caregivers are women; more specifically, over one-third of dementia caregivers are daughters.
- Most caregivers (66%) live with the person with dementia in the community.
- Approximately one-quarter of dementia caregivers are "sandwich generation" caregivers — meaning that they care not only for an aging parent but also for at least one child.
Alzheimer's takes a devastating toll on caregivers. Compared with caregivers of people without dementia, twice as many caregivers of those with dementia indicate substantial emotional, financial and physical difficulties.
Of the total lifetime cost of caring for someone with dementia, 70% is borne by families — either through out-of-pocket health and long-term care expenses or from the value of unpaid care.
Caring for someone living with Alzheimer's?
Get the support you need to handle the day-to-day, plan for the future and help you live well.
Workforce
 As the prevalence of Alzheimer's disease increases, so does the need for more members of the paid workforce to be knowledgeable and skillful about working with a diverse population of people living with dementia, as well as with their families.
As the prevalence of Alzheimer's disease increases, so does the need for more members of the paid workforce to be knowledgeable and skillful about working with a diverse population of people living with dementia, as well as with their families.
- Fifty-five percent of primary care physicians (PCPs) caring for people living with Alzheimer's report there are not enough dementia care specialists in their communities.
- Between 2021 and 2031, more than 1 million additional direct care workers will be needed to care for the growing population of people living with dementia — the largest worker gap of any single occupation in the U.S.
- Half of PCPs reported that they do not feel adequately prepared to care for individuals with Alzheimer's and other dementias.
- The U.S. will have to nearly triple the number of geriatricians to effectively care for the number of people projected to have Alzheimer's in 2050.
- Turnover rates for direct care workers are high — estimated at 77% annually for those providing home care and 99% for nursing assistants in nursing homes.
Be prepared and talk to your doctor
Effective communication with your doctor is important when you are seeking a diagnosis for memory loss. Be prepared to ask questions and be as honest as possible.
Costs of health care
 The costs of health care and long-term care for individuals living with Alzheimer's or other dementias are substantial, and dementia is one of the costliest conditions to society.
The costs of health care and long-term care for individuals living with Alzheimer's or other dementias are substantial, and dementia is one of the costliest conditions to society.
In 2024, health and long-term care costs for people living with Alzheimer's and other dementias are projected to reach $360 billion — not including the value of unpaid caregiving. Medicare and Medicaid are expected to cover $231 billion (64%), while out-of-pocket spending is expected to be $91 billion. Total payments for health care, long-term care and hospice care for people living with dementia are projected to increase to nearly $1 trillion in 2050.
- The total lifetime cost of care for a person living with dementia is estimated at almost $400,000. Seventy percent of these costs are borne by family caregivers in the forms of unpaid caregiving and out-of-pocket expenses.
- People living with Alzheimer's or other dementias have twice as many hospital stays per year as other older people.
- Medicare beneficiaries with Alzheimer's or other dementias are more likely than those without dementia to have other chronic conditions, such as heart disease, diabetes and kidney disease.
- Older people living with Alzheimer's or other dementias have more skilled nursing facility stays and home health care visits per year than other older people.
- People living with Alzheimer's or other dementias make up a large proportion of all elderly people who receive adult day services and nursing home care.
Take action
Ending Alzheimer's is possible — Congress can make it happen. Join us and help make Alzheimer's a national priority.
Special Report — Mapping a Better Future for Dementia Care Navigation
 Dementia care is a complex maze with interactions between primary care providers, specialists, social services, medication management and caregiver support. Navigating this maze is difficult and often frustrating for people living with Alzheimer's or other dementia and their caregivers. Without a clear path forward, any roadblock or detour along the way can have considerable consequences — whether they be missed opportunities for treatment, missed connections to resources and services, or missed chances for maintaining quality of life.
Dementia care is a complex maze with interactions between primary care providers, specialists, social services, medication management and caregiver support. Navigating this maze is difficult and often frustrating for people living with Alzheimer's or other dementia and their caregivers. Without a clear path forward, any roadblock or detour along the way can have considerable consequences — whether they be missed opportunities for treatment, missed connections to resources and services, or missed chances for maintaining quality of life.
Mapping a Better Future for Dementia Care Navigation (PDF) provides a comprehensive look at dementia care navigation, a holistic model of care that provides medical and social support for people living with dementia and their caregivers in order to alleviate stress, improve health outcomes and lower costs. Dementia care navigation emphasizes person-centered, evidence-based, culturally competent, empowered support throughout the dementia care journey. Support services include:
- Caregiver education and training.
- Care coordination, including scheduling appointments, coordinating diagnostic testing, and facilitation communication and referrals across specialities and organizations.
- Connecting people living with dementia and caregivers to education and training, social services, and community support.
- Management of chronic conditions, medication, symptoms and dementia-related behaviors.
- Safety assessments.
- Advance care planning.
- Assistance with insurance and benefits.
Overwhelmingly, caregivers would welcome dementia care navigator support and believe it would benefit both the person living with dementia and the caregiver.
- Seven in 10 dementia caregivers say that coordinating care is stressful.
- More than 4 in 5 dementia caregivers (85%) say having access to a care navigator would influence their choice of dementia health care provider for the person they care for.
- Three in 5 dementia caregivers (61%) believe that having a care navigator would improve quality of life for their care recipient, and 43% believe that a care navigator would improve the care recipient's overall health.
- Three in 5 dementia caregivers say less stress (62%) and more peace of mind (62%) would be valuable outcomes of having a care navigator. More than half (56%) say having a care navigator could help them be better caregivers.
The special report national survey also found that 60% of health care workers believe that the U.S. health care system is not effectively helping patients and their families navigate dementia care.
The special report survey revealed three recommendations for health care systems to advance dementia care navigation efforts:
- Formalize the dementia care navigator role and increase navigator proficiency in dementia care.
- Scale and expand access to dementia care navigation programs.
- Create direct lines to dementia care navigators, such as a 24/7 helpline.
Health care delivery that includes dementia care navigation can improve the quality of life of those facing dementia and their caregivers, paving the way for a more sustainable, efficient and compassionate health care system. Learn more in Mapping a Better Future for Dementia Care Navigation (PDF) and view the special report infographic (PDF).
For more information about dementia care navigation, read the Dementia Care Navigation Guiding Principles, a national framework for dementia care navigation within or in collaboration with U.S. health systems, and consider participating in the Dementia Care Navigation Roundtable.
Read past special reports
Call our free 24/7 Helpline (800.272.3900)
Talk to a dementia expert now and get confidential emotional support, local resources, crisis assistance and information in over 200 languages. It's ok if you don't know where to start. Just give us a call and we'll guide you from there.