Some researchers fight Alzheimer’s in and out of the lab
For some dementia researchers, the motivation to end Alzheimer’s disease isn’t just professional — it’s personal.
While pursuing careers as scientists and clinicians, Dorene Rentz, Psy.D., Oanh Meyer, Ph.D., and Luis D. Medina, Ph.D., felt the weight of their work at home when family members developed Alzheimer’s. For each, the experience has only strengthened their resolve to better understand the disease and improve the lives of everyone affected.
Dorene Rentz, Pys.D.
A neuropsychologist for over 30 years, Dorene Rentz, Psy.D., has a deep knowledge of Alzheimer’s disease and its signs. When her mother-in-law, Sheila, showed symptoms of cognitive decline in the late 1990s, Rentz asked Sheila’s primary care doctor to evaluate her for Alzheimer’s. Convinced that Rentz, a professor at Harvard Medical School, was just an “East Coast know-it-all,” the doctor initially rejected such a diagnosis — only to call Rentz and her husband six months later concerned that Sheila could no longer function on her own.
“It was so obvious to me that she had Alzheimer’s,” Rentz says. “In the span of a few days, we moved her from Florida to Boston to live with us. That was the beginning of my front-row seat, living day-to-day with the disease.”
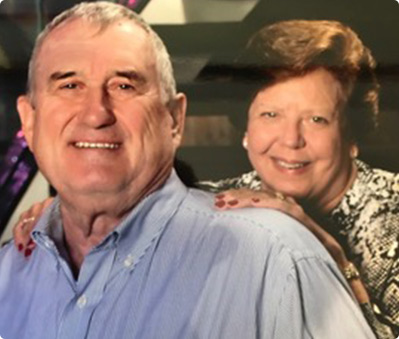
Sheila died in 2003. Despite Rentz’s familiarity with the disease, when her husband, Ray, started displaying signs of cognitive decline around 2015, Rentz experienced the same denial that strikes so many unsuspecting families. She disregarded or excused many of his memory problems until the overlap of her career and personal life brought reality to the surface.
Professionally, she was recruiting people for a landmark clinical trial, the Anti-Amyloid Treatment in Asymptomatic Alzheimer’s Study (A4 Study). She knew it was time to consider Ray as a candidate.
This is a time of unprecedented promise in the quest to end Alzheimer’s. The Alzheimer's Association is growing philanthropic support for research, fostering a dynamic community of scientists and securing increased federal funding.
Find Out How
“I sat him down and said, ‘We need to consider enrolling you in this trial.’ He passed the screening for the A4 Study,” she says. “The good news was he qualified for enrollment. The bad news was that this meant his brain was burdened with beta-amyloid plaques [a hallmark brain change of Alzheimer’s disease].”
While Ray is currently managing the disease well, Rentz continues to notice changes — for example, Ray’s once jovial spirit has dimmed. While the changes bring sadness, they also provide perspective.
“I can now intimately relate to my patients who are facing dementia,” says Rentz, who continues her clinical work today. “I sometimes share that my husband has early-stage Alzheimer’s, which adds credibility to what I’m saying and that I have their best interests at heart.”
Oanh Meyer, Ph.D.

As a Vietnamese American and social psychologist, Oanh Meyer, Ph.D., felt a calling to study how underserved populations are disproportionately affected by cognitive and mental health issues. In 2013, as she started researching how social factors may impact Asian Americans’ risk of developing Alzheimer’s, she began noticing memory changes in her own mother.
“After going through the whole diagnosis and care planning process with my mother, I was struck by how difficult it was — and I was born in the United States, understand the health care system and speak English fluently,” says Meyer, an assistant professor of neurology at the University of California, Davis. “I realized how challenging it must be for individuals who can’t advocate for themselves or have to navigate cultural or language differences. That experience motivated me to help caregivers understand what they’re going through.”
According to the Alzheimer’s Association
2021 Alzheimer’s Disease Facts and Figures report, 30% of Asian-American caregivers say they have faced discrimination when navigating health care settings for their care recipients. Moreover, 23% of Asian-American caregivers have cited language as a barrier to care.
To help tackle this challenge, Meyer received an Alzheimer’s Association research grant that explores the issues faced by Vietnamese American dementia caregivers. In this project, Meyer took an existing caregiver stress aid and adapted it into a culturally relevant program that enhances care practices for Vietnamese Americans.

“In Vietnamese, your last name is said or listed before your first name,” Meyer explains. “So it can be confusing for caregivers in the U.S. when their name is called at a doctor’s office or when filling out paperwork. It’s something minor, but those little idiosyncratic things really complicate the process for caregivers if they don’t know what to expect.”
As her mother’s caregiver, Meyer brings real-life experience to her work every day — and finds her own sense of comfort within the caregiving community she studies.
“Would I wish my mom to have Alzheimer’s so I can study this? No, of course not,” she says. “But I guess the silver lining is that it’s really helped me have a lot of compassion for the people involved in my research and better understand the results I see.”
Luis D. Medina, Ph.D.

Luis D. Medina, Ph.D., began his research career analyzing how cultural factors impact the brain and behavior. As a first-generation Puerto Rican, as well as a bilingual psychologist and cultural neuropsychologist, Medina recognized the potential impact he could have working with underrepresented populations facing dementia. He would come to learn firsthand the importance of his research.
“Alzheimer’s has struck my family hard and, unfortunately, more than once,” says Medina, director of the Collaborative on Aging Research and Multicultural Assessment at the University of Houston. “Even for those of us who study the disease, it doesn’t make the experience any less painful.”
Medina’s maternal grandmother was diagnosed with Alzheimer’s shortly before he began his doctorate work in 2009. His mother and six aunts shared the caregiving responsibilities until Medina’s grandmother died in 2012. Shortly after, two of his aunts developed dementia.

Hispanics are about one-and-a-half times as likely as older Whites to have Alzheimer’s or another dementia, but there still isn’t enough research to explain why. Medina started the Collaborative on Aging Research and Multicultural Assessment to study the full clinical picture of the disease in Hispanic communities. With funding from the Alzheimer’s Association and the National Institutes of Health, he is currently exploring how to improve diagnostic tools for Hispanic people and is developing strategies to increase their recruitment into research studies.
“A large part of this work has shown me that we don’t really separate our professional lives from our personal ones,” Medina says. “When you’re able to share that [Alzheimer’s] is your hardship, too, it helps bridge a lot of the communication gaps that have existed between these communities and research institutions. It builds trust, which is so important.”